Analysis of cell-free DNA in maternal blood in screening for aneuploidies: updated meta-analysis
ABSTRACT
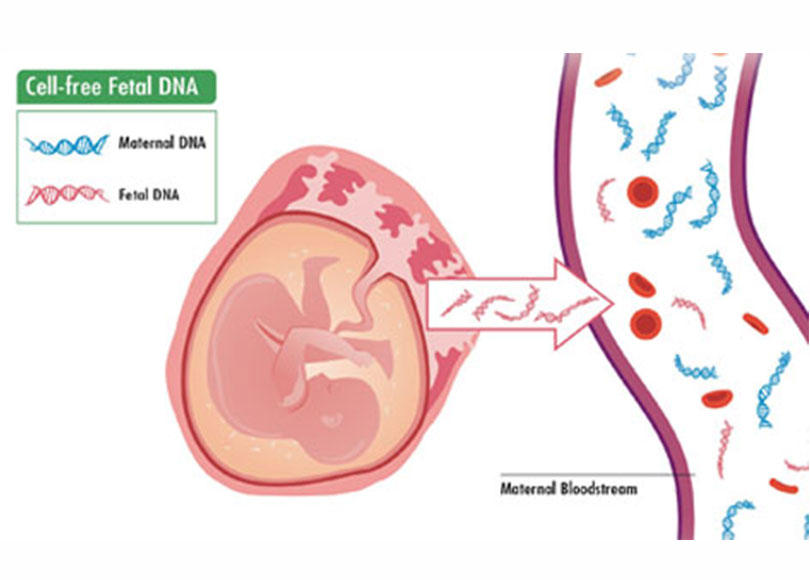
Objectives To review clinical validation or implementation studies of maternal blood cell-free (cf) DNA analysis and define the performance of screening for fetal trisomies 21, 18, and 13 and sex chromosome aneuploidies (SCA).
Methods Searches of PubMed, EMBASE, and The Cochrane Library were performed to identify all peer-reviewed articles on cfDNA testing in screening for aneuploidies between January 2011, when the first such study was published, and 31 December 2016. The inclusion criteria were a peer-reviewed study reporting on clinical validation or implementation of maternal cfDNA testing in screening for aneuploidies, in which data on pregnancy outcomes were provided for more than 85% of the study population. We excluded case–control studies, proof-of-principle articles, and studies in which the laboratory scientists carrying out the tests were aware of fetal karyotype or pregnancy outcome. Pooled detection rates (DRs) and false-positive rates (FPRs) were calculated using bivariate random-effects regression models.
Results In total, 35 relevant studies were identified and these were used for the meta-analysis on the performance of cfDNA testing in screening for aneuploidies. These studies reported cfDNA results in relation to fetal karyotype from invasive testing or clinical outcome. In the combined total of 1963 cases of trisomy 21 and 223 932 non-trisomy 21 singleton pregnancies, the weighted pooled DR and FPR were 99.7% (95% CI, 99.1–99.9%) and 0.04% (95% CI, 0.02–0.07%), respectively. In a total of 563 cases of trisomy 18 and 222 013 non-trisomy 18 singleton pregnancies, the weighted pooled DR and FPR were 97.9% (95% CI, 94.9–99.1%) and 0.04% Correspondence to: Prof. K. H. Nicolaides, Fetal Medicine Research Institute, King’s College Hospital, 16–20 Windsor Walk, Denmark Hill, London SE5 8BB, UK (e-mail: kypros@fetalmedicine.com)
Accepted: 3 April 2017
(95% CI, 0.03–0.07%), respectively. In a total of 119 cases of trisomy 13 and 212 883 non-trisomy 13 singleton pregnancies, the weighted pooled DR and FPR were 99.0% (95% CI, 65.8–100%) and 0.04% (95% CI, 0.02–0.07%), respectively. In a total of 36 cases of monosomy X and 7676 unaffected singleton pregnancies, the weighted pooled DR and FPR were 95.8% (95% CI, 70.3–99.5%) and 0.14% (95% CI, 0.05–0.38%), respectively. In a combined total of 17 cases of SCA other than monosomy X and 5400 unaffected singleton pregnancies, the weighted pooled DR and FPR were 100% (95% CI, 83.6–100%) and 0.004% (95% CI, 0.0–0.08%), respectively. For twin pregnancies, in a total of 24 cases of trisomy 21 and 1111 non-trisomy 21 cases, the DR was 100% (95% CI, 95.2–100%) and FPR was 0.0% (95% CI, 0.0–0.003%), respectively.
Conclusions Screening by analysis of cfDNA in maternal blood in singleton pregnancies could detect >99% of fetuses with trisomy 21, 98% of trisomy 18, and 99% of trisomy 13 at a combined FPR of 0.13%. The number of reported cases of SCA is too small for an accurate assessment of the performance of screening. In twin pregnancies, the performance of screening for trisomy 21 is encouraging but the number of cases reported is small.






