Contingent first-trimester screening for aneuploidies with cell-free DNA in a Danish clinical setting
ABSTRACT
Objectives
The primary aim of this study was to compare the screening performance for trisomy 21 (T21) between combined first-trimester screening (cFTS) with referral for invasive testing at a T21 risk ≥ 1 in 300, and contingent screening consisting of referral for invasive testing at a cFTS-T21 risk ≥ 1 in 100 and referral for cell-free DNA (cfDNA) testing at a cFTS-T21 risk between 1 in 100 and 1 in 1000. Secondary aims were to compare the incidence of fetuses diagnosed with trisomy 18 (T18), trisomy 13 (T13) or sex chromosome aneuploidy, and examine the association between fetal fraction of cfDNA in maternal blood and maternal/fetal characteristics.
Methods
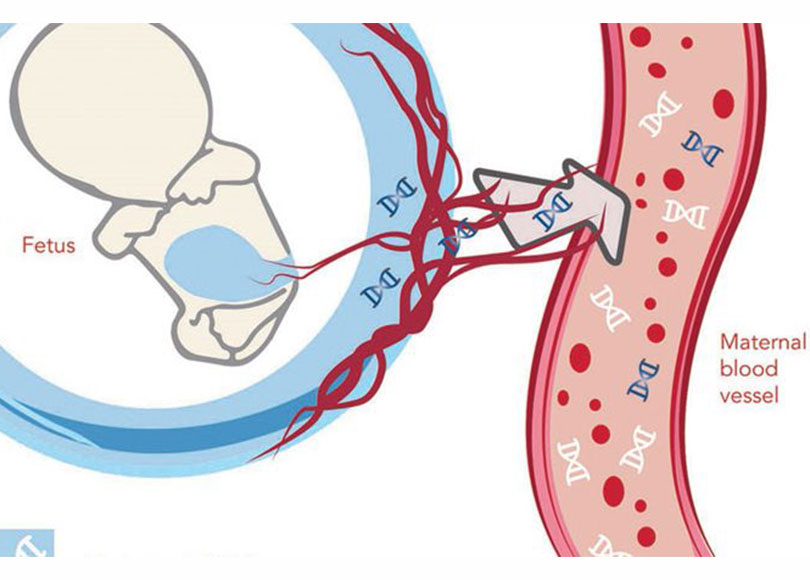
Women with a singleton pregnancy and a cFTS-T21 risk of ≥ 1 in 1000 were recruited consecutively from two Danish hospitals between August 2014 and May 2015. First-trimester combined screening was based on maternal age, nuchal translucency thickness and levels of pregnancy-associated plasma protein A (PAPP-A) and β-human chorionic gonadotropin (β-hCG). Blood samples for cfDNA testing were analyzed for risks of T21, T18, T13 and sex chromosomal aneuploidies. cfDNA analysis was conducted blinded to the cFTS assessment and karyotype results. Pregnancy outcomes and pre- and postnatal karyotypes were obtained from the Danish Fetal Medicine Database.
Results
Among 6449 women who underwent cFTS risk assessment, 869 (13.5%) had a T21 risk of ≥ 1 in 1000 and 597 were included for cfDNA testing. Among these, there were 15 cases of T21, one case of T18 and two cases of T13. The sensitivity for detection of T21 was Correspondence to: Dr C. B. Miltoft, Center of Fetal Medicine, Department of Obstetrics, Copenhagen University Hospital, Rigshospitalet, Blegdamsvej 9, 2100 Copenhagen, Denmark (e-mail: miltoft@dadlnet.dk) Accepted: 13 June 2017 100% using both screening strategies, while specificity increased significantly (P < 0.0001) from 97.0% using the cFTS strategy to 98.8% using the contingent approach. The sensitivity for detection of T21, T18 and T13 increased from 94.4% using the cFTS strategy to 100% using the contingent approach, with overlapping CIs, while specificity increased significantly (P < 0.0001) from 97.1% for cFTS to 98.9% for the contingent strategy. Seven pregnancies were categorized as being at increased risk of a sex chromosomal aneuploidy by cfDNA testing but chromosome analysis was discordant, corresponding to a false-positive rate of 1.2%. The fetal fraction decreased significantly with increasing maternal weight and increased significantly with the level of β-hCG and PAPP-A and among female fetuses, in both univariate and multivariate analyses.
Conclusions
In a clinical setting with efficient cFTS, contingent screening offering women with a cFTS risk of ≥ 1 in 100 an invasive test and women with a risk from 1 in 100 to 1 in 1000 a cfDNA test had the same sensitivity for T21, T18 and T13, but significantly increased specificity, when compared with offering an invasive test to all women with a risk of ≥ 1 in 300. Implementing contingent screening would therefore reduce significantly the number of invasive tests performed at no loss of sensitivity.






